Winter 2016: Energy Evolution
From carbon dioxide conversion to landfill mining, researchers at UTA are seeking viable alternative energy options.
Skip to content. Skip to main navigation.
From carbon dioxide conversion to landfill mining, researchers at UTA are seeking viable alternative energy options.
Found in everything from space shuttles to dental fillings, composite materials have thoroughly infiltrated modern society. But their potential is still greatly untapped, offering researchers ample opportunity for discovery.
Within the particle showers created at the Large Hadron Collider, answers to some of the universe’s mysteries are waiting.
Model systems like pigeons can help illuminate our own evolutionary and genomic history.
UT Arlington's tiny windmills are bringing renewable energy to a whole new scale.
The stability of our highways, pipelines, and even manholes is reaching a breaking point.
Scientists believe they have discovered a subatomic particle that is crucial to understanding the universe.
UT Arlington researchers unlock clues to the human body’s most mysterious and complex organ.
UT Arlington researchers probe the hidden world of microbes in search of renewable energy sources.
Wounded soldiers are benefiting from Robert Gatchel’s program that combines physical rehabilitation with treatment for post-traumatic stress disorder.
Tiny sensors implanted in the body show promise in combating acid reflux disease, pain and other health problems.
Nanotechnology researchers pursue hybrid silicon chips with life-saving potential.
Biomedical engineers combat diseases with procedures that are painless to patients.
Photograph By Gallery Stock
The human body has ways of fighting foreign invaders. The immune system’s vast network of cells, tissues, and organs works to neutralize pathogens like bacteria or viruses and remove them from the body. It also recognizes harmful environmental substances and provides defenses, such as sneezing. But what happens if the invader isn’t so foreign?
Cancer is a threat that starts from within, when abnormal cells divide uncontrollably and run amok. While some cells of the immune system can help fight cancer, their efforts more often than not aren’t enough to eradicate the insidious—and devastating—disease.
That devastation can be seen in the statistics. The National Cancer Institute estimated that 1,685,210 new cases of cancer were diagnosed in the United States in 2016, with 595,690 people dying from the disease. Overall, 39.6 percent of the country’s population is expected to develop cancer at some point during their lifetimes, with national expenditures for cancer care reaching $156 billion in 2020.
But at The University of Texas at Arlington, a major change is stirring. As researchers work tirelessly to attack cancer from all angles, their discoveries are advancing beyond the theoretical and into the actual as they move from the lab to the commercial sector. Their work has already had a tangible impact on cancer care—and it’s only the beginning.
Some of the biggest impact comes from research being done in immunotherapy. Designed to boost the body’s natural defenses to fight cancer, immunotherapy can slow or even stop the growth of cancer cells and prevent the disease from spreading to other parts of the body. At UTA, researchers working in this area are successfully commercializing next-generation cancer therapies.
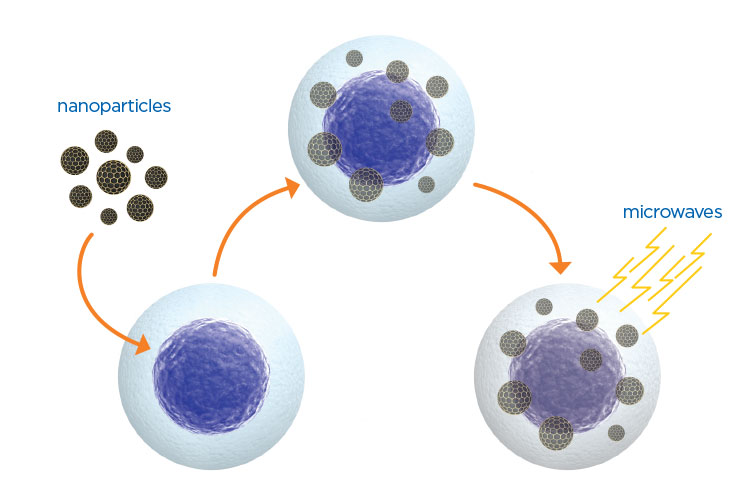
A study by Wei Chen demonstrated that copper cysteamine nanoparticles can be activated by microwaves, then targeted directly at a tumor
A major figure in immuno-oncology research is Jon Weidanz, UTA’s associate vice president for research and a professor of biology. His company, AbeXXa Biologics, is developing antibody drugs that can target specific proteins on cancer cells. The company also signed a significant collaboration agreement with a large pharmaceutical company to develop next-generation therapeutic agents for cancer immunotherapy.
“Further facilitating the translation of our inventions into viable therapies—with investment backing from major pharmaceutical companies, corporate venture capital, and angel investors—is an important strategy as we move forward,” Dr. Weidanz says. “This will allow us to create an innovation hub around cancer that will integrate the University with surrounding businesses.”
In another immunotherapy advancement, biochemists have demonstrated the mechanism behind how thiopurine drugs suppress immune response. While effective in treating cancer, these drugs can cause side effects like cardiovascular disease and hypertension.
The researchers, led by Jongyun Heo, associate professor of chemistry, showed that thiopurine drugs create a disulfide bond with the Rac1 proteins within the immune system’s T cells. This bond deactivates the protein and suppresses the cell’s immune response. Dr. Heo’s study also demonstrated that thiopurine can form bonds with other proteins in T cells like RhoA, which is involved in vascular functions, and Cdc42, whose aberrant activation can result in cancerous growths.
Most people are familiar with the more traditional method of treating cancer, chemotherapy—and with its debilitating side effects. UTA researchers are working on ways to improve chemical therapies to help patients live healthier, happier lives throughout treatment.
To that end, Fred MacDonnell, chair of the Chemistry and Biochemistry Department, co-founded Tuevol Therapeutics, a company that has exclusively licensed the intellectual property to TS101, a ruthenium-based metallodrug that shows effectiveness against platinum-resistant lung cancer. Ruthenium is a rare metallic element, and the drug developed at UTA has many of the therapeutic effects of platinum-based drugs, but without the side effects. Rolf Brekken and Tom Wilkie of the UT Southwestern Hamon Center for Therapeutic Oncology are co-founders and are working with Dr. MacDonnell to advance this drug to clinical studies.
In a development that could transform cancer treatment, physics Professor Wei Chen was lead author on a study demonstrating that using microwaves to activate photosensitive nanoparticles produces tissue-heating effects that ultimately lead to cell death within solid tumors. This groundbreaking combination of microwaves and photodynamic therapy (commonly used to treat skin cancers) could open new ways to target deeply situated tumors.
“Our new microwave-induced photodynamic therapy offers numerous advantages, the most significant of which is increased safety,” Dr. Chen explains. “Our copper cysteamine nanoparticle also demonstrates very low toxicity, is easy to make, is inexpensive, and emits intense luminescence, which means it can also be used as an imaging agent.”

Jon Weidanz’s company is developing therapeutic agents to stop cancer growth
The researchers demonstrated that both in vitro and in vivo studies on an osteosarcoma cell line showed significant cell destruction using copper cysteamine nanoparticles under microwave activation. The heating effects and the release of copper ions from copper cysteamine upon activation was the main mechanism for the generation of the reactive oxygen needed for cancer cell destruction.
Chen was joined on this project by UTA physics research Assistant Professor Lun Ma, as well as Mengyu Yao, Lihua Li, and Yu Zhang from the Guangdong Key Laboratory of Orthopaedic Technology and Implant Materials; and Junying Zhang from Beihang University. Their findings were published in The Journal of Biomedical Nanotechnology.
“Dr. Chen’s research into nanoparticle activation has led to important discoveries that could potentially transform cancer treatment,” says Alex Weiss, chair of the Physics Department. “This new paper on the possibilities of microwave activation demonstrates yet again how his search for new modalities of therapy could play a key role in finding safe, viable, and inexpensive treatments for cancer.”
Whether a cancer patient is in treatment or in remission, quality of life is a consistent concern. Studies have shown that cancer patients who exercise during and after treatment improve their cardiorespiratory fitness and quality of life. Further, pre-clinical studies suggest that if patients exercise during treatment, chemotherapy may be more effective in targeting cancer cells.
A team led by Jongyun Heo showed how thiopurine drugs suppress immune response
In 2016, the College of Nursing and Health Innovation teamed with the Cancer Foundation for Life to bring FitSTEPS for Life to campus. FitSTEPS is a free, community-based nutrition and exercise program designed to help cancer patients increase mobility and boost endurance while undergoing treatment. The program is structured, tailored to the individual, and includes aerobic exercise, strength training, and stretching techniques. It is designed to mitigate the debilitating effects of chemotherapy and radiation.
Mark Haykowsky, the Moritz Chair of Geriatric Nursing and Research, leads the program.
“A community’s greatest asset is a healthy, thriving population,” says Anne Bavier, dean of the College of Nursing and Health Innovation. “Partnerships of this kind help ensure better survival rates for cancer patients in our community. They also help ensure a better quality of life. Helping tackle such real-life problems is a critically important part of our reason for being as a health-focused college and as a University.”
While researchers at UTA are collectively working to eradicate this pernicious disease once and for all, the University continues to evolve into a major hub for cancer research. Last year showed major growth in this realm, with key recruits in cancer research joining the faculty and $6 million in new grants received to develop cancer-fighting technologies. UTA also broke ground on the Science and Engineering Innovation and Research building, which will be the center of life and health science teaching and research on campus when it opens in 2018.
“UTA’s scientific expertise in basic cancer research, identification, and diagnostics, and in noninvasive, mid-term, invasive, and post-operative therapies is accelerating dramatically in order to enable substantial impact on the health of Texas,” says President Vistasp Karbhari. “By assembling a world-class team, we hope not only to make transformative advances in key areas related to cancer, but also to provide the highest level of educational and research experiences to our students.”