With 208 bones, 650 muscles, about 1,300 tendons, and a multitude of vessels and nerves, the musculoskeletal system is the largest system in the human body. A group of researchers at The University of Texas at Arlington is dedicated to studying this intricate system and solving its mysteries—especially as they relate to chronic disease and aging.
“We want to understand the musculoskeletal system, answer essential questions about its mechanisms, and discover strategies for improved function during development and aging to determine new strategies for healing,” says Marco Brotto, the George W. and Hazel M. Jay Endowed Professor in the College of Nursing and Health Innovation.
He heads the new Bone-Muscle Research Center (BMRC), which features the work of seven researchers with different areas of expertise in bone, muscle, neuronal, and vascular biology.
In addition to Dr. Brotto, the BMRC comprises Rhonda Prisby, head of the Bone Vascular and Microcirculation Laboratory; Dan Trott, whose expertise is integrative immunology; Venu Varanasi, who focuses on bone-muscle regeneration; Zui Pan, an expert in calcium signaling in cancer, muscle aging, and cardiovascular disorders; and Jingsong Zhou, whose recent research covers amyotrophic lateral sclerosis (ALS) and aging muscle disorders. The researchers also have individual labs.
Although they are each driven by different experiences and motivations, their overall goal is the same: to find answers and solutions for better health outcomes.
“We are applied, basic, translational, and clinical scientists working together with chemists, engineers, and computational biologists to find new answers to old and new questions,” Brotto says. “We’re using highly innovative, integrative, and transdisciplinary approaches to find new cures and promote longer and healthier living.”
Growing Older, Not Stronger
As people grow older, the density of their bones lessens. Consequently, bones become more delicate and easier to break.
“We are living longer, but are seeing many chronic problems,” says Brotto. “As people age, especially if they lead sedentary lifestyles, they continuously lose mass and function of their musculoskeletal system, which can lead to developing conditions such as atherosclerosis, osteoporosis, and sarcopenia.”
Compounding this problem is the projected growth of our older population. In less than two decades—and for the first time in U.S. history—older adults will outnumber children. Helping this demographic stay healthy is thus becoming ever more critical.
It is crucial to seek solutions to further advance the health and quality of life for this rapidly growing population.
“The key focus of our center is to detect aging-related problems in someone’s 30s or 40s, not their 60s or 70s,” Brotto says. “We want to tackle problems before it’s too late.”
Nearly 128 million people in the United States and 2 billion worldwide currently suffer from musculoskeletal conditions. These often-devastating ailments can significantly reduce quality of life and annually cost $1 trillion to treat in the U.S.
To help reduce these numbers, Brotto is using a series of National Institutes of Health (NIH) grants totaling approximately $6.575 million to tackle a variety of musculoskeletal diseases. His projects include determining how bone cells can influence and change the function of muscles by releasing hormone-like molecules, examining the mechanisms that contribute to the loss of strength in muscle during aging, determining if regulating certain proteins can improve the function of aged skeletal muscles, investigating the role of a protein called “numb” in muscle function and weakness with aging, and working to develop protein gene activators to protect skeletal muscles from diabetes.
“The outcome of this work could significantly enhance the quality of life for older adults,” says Kathryn Daniel, associate professor of nursing and director of the Adult Gerontology Primary Care Nurse Practitioner program. “It is crucial to seek solutions to further advance the health and quality of life for this rapidly growing population.”
Muscle Atrophy and ALS
BMRC Associate Director Jingsong Zhou’s research focuses on a different form of musculoskeletal disorder: ALS, more commonly referred to as Lou Gehrig’s disease. The majority of research on ALS centers on the spinal cord because of how the disease affects neurological function. But Dr. Zhou is investigating the theory that ALS affects the physiology of the whole body through defective cells in multiple organs.
“In the beginning, we believed the muscle atrophy ALS causes was secondary to the death of the neurons in the spinal cord, but we have evidence that indicates the muscle is not only a victim of the disease, but also it actively contributes to it,” says Zhou, who is also a professor of kinesiology. “This is a systemic disorder affecting the whole body.”
She recently received a $2.88 million award from the NIH to preserve mitochondria as they function or dysfunction in a diseased cell. This will help clarify the mechanisms behind why multiple organs are involved in ALS deterioration.
“We are ultimately working to find some potential therapeutic means to treat the disease with a new understanding,” Zhou says. “Once we understand why the cells are damaged, we can test potential compounds or therapies.”
Different Perspectives
Two other bone-muscle researchers are using their unique backgrounds to help inform their work.
Kinesiology Associate Professor Rhonda Prisby earned an undergraduate degree in art, an education that she believes has enabled her to see science from a unique vantage point.
“I have found that art and science share similar traits,” she says. “Like art, research allowed me to come up with my own ideas, be creative, and ask what if?”
With this honed, artistic eye, she was able to notice something important lurking in the blood vessels within bone marrow.
“By examining seemingly unrelated images and linking the details of them together, I was able to posit the presence of bone-like particles in the blood,” Dr. Prisby explains. “In fact, some of the ossified particles are large enough to clog the smallest blood vessels in the vascular tree.”
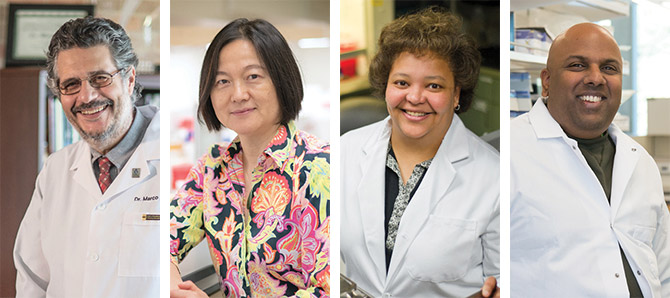
From left: Marco Brotto, Jingsong Zhou, Rhonda Prisby, and Venu Varanasi are exploring the musculoskeletal system.
While vascular calcification—mineral deposits on the walls of arteries and veins—is a common characteristic and risk factor for morbidity and mortality, Prisby’s bone-like particles are potentially more dangerous because of their sharp edges.
“Some of the ossified particles have sharp tips and edges that could damage the lining of blood vessels,” she says. “This damage could initiate events leading to atherosclerosis—or a build-up of plaque—which can restrict blood flow over time.”
The discovery of these particles could help physicians detect and treat potentially life-threatening conditions such as heart attack, stroke, and inadequate blood supply to the limbs.
Unlike Prisby, Venu Varanasi’s unique perspective comes not from his education, but from his genes. As a child, the associate professor of nursing was diagnosed with a genetic retinal disorder that has slowly deteriorated his vision. Problems with his eyesight first began to affect his career as a postdoctoral fellow at the University of California at San Francisco, leaving him unable to perform the precise microscopic measurements his work demanded.
Although he could have given up or pursued a different path, Dr. Varanasi instead chose to adapt, training his students to handle the micro-level, precise movements his research requires.
“There is an inherently collaborative atmosphere in Dr. Varanasi’s lab,” says Neelam Ahuja, a doctoral student who works as Varanasi’s faculty associate. “He empowers us to be equal players in the research.”
Much of this research is focused on severe cranium injuries, which often have difficulty healing due to the large size of the missing bone. While metal or plastic implants are a solution, they can take a long time to be tailored to fit and support bone fixation.
As an alternative, Varanasi and his team developed a method for live 3D printing of bone-forming scaffolds in the cranium that are grafted to bone defects in real-time. This non-invasive approach would lead to shorter healing times and be more in tune with the body’s natural healing processes.
“We have the potential to change the way we deliver health care,” Varanasi says. “We’re moving past current methods of cutting and patching patients and building a transformative method that will heal them without invasive techniques. Our research could have implications for healing fractures in aging adults as well as potential applications for healing muscle loss.”
Brotto believes Varanasi’s work marks a bold, new approach to the treatment of musculoskeletal maladies.
“Venu’s work captures the meaning of translational research and has tremendous commercialization potential,” he says. “Implants for cranial defects require continued care and medical attention, which leads to high costs for the patient. Venu’s research could bring about a new family of devices that promote self-healing, which not only is the best way for a patient to heal, but also leads to increased accessibility of treatment.”